Indications for safe and effective regenerative therapy using allogeneic transplantation of iPS-cell-derived DA progenitors
There is still much to investigate about the safety and efficacy of iPS-cell-derived cell products. After bilateral putaminal transplantation, the average motor severity was decreased and the mean 18F-DOPA uptake was increased at the 24-month follow-up. Despite the abovementioned limitations, these findings suggest that allogeneic transplantation of iPS-cell-derived DA progenitors is a safe and effective regenerative therapy for patients with PD. Future strategies may combine cell transplantation with gene therapy, medication and rehabilitation to enhance efficacy44. Moreover, as demonstrated in a single case study8, autologous transplantation using iPS cells may also be a promising option.
The studies, published by two groups in Nature today, are “a big leap in the field”, says Malin Parmar, a stem-cell biologist at Lund University, Sweden. The cell products are safe and have signs of survival.
The trials were only meant to test safety and were less than 20 people, which was not enough to determine the effectiveness of the intervention.
“Some people got slightly better and others didn’t get worse,” says Jeanne Loring, a stem-cell researcher at Scripps Research in La Jolla, California, which could be due to the relatively small number of cells transplanted in these first early-stage trials.
A dose of 0.9 million stem cells for Parkinson’s disease in the United States and the European registry of dopamine-producing neurons in the human brain
Parkinson’s is a progressive neurological condition driven by the loss of dopamine-producing neurons, which causes tremors, stiffness and slowness in movement. There is currently no cure for the condition, which is projected to affect 25 million people globally by 2050.
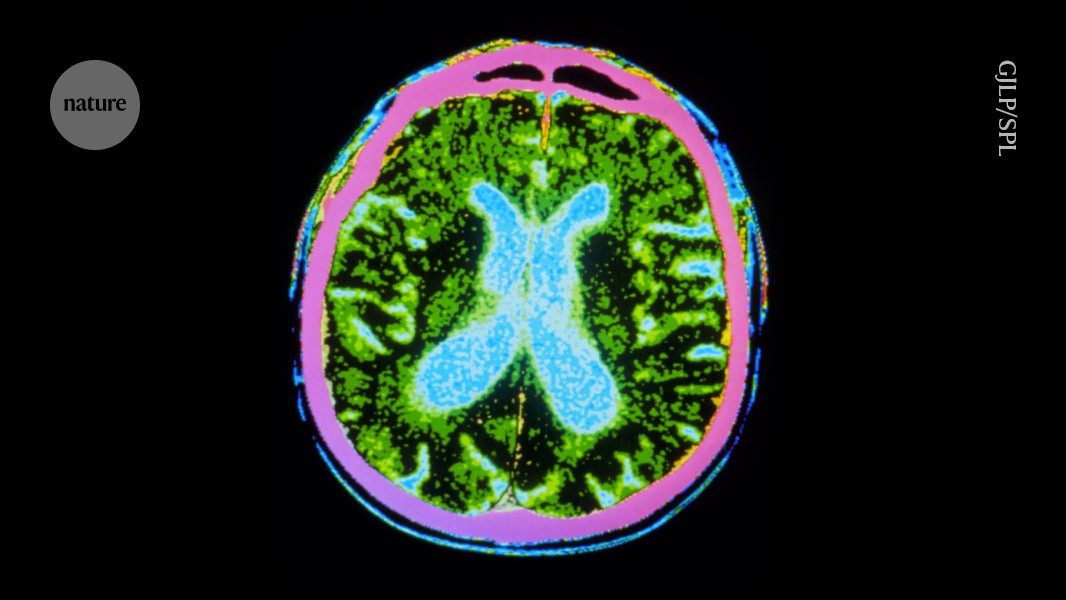
The stem cells were injected to 18 sites across the putamen in both hemispheres — “to roughly fill up that region of the brain”, says Viviane Tabar, a neurosurgeon at the Memorial Sloan Kettering Cancer Center in New York City who conducted the US surgeries.
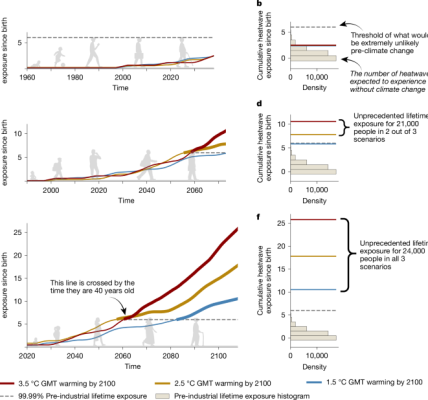
It was hoped that 100,000 and 300,000 cells, respectively, would survive the surgery, so that 5 individuals received a dose of 0.9 million cells. A healthy brain typically has 300,000 dopamine-producing neurons. The recipients were given immune-suppressing drugs for one year after the surgery to prevent their bodies from rejecting the transplant.
Brain scans showed an increase in dopamine production, indicating that some of the brain cells still existed after receiving immune-suppressing drugs.
On average, individuals who received the low dose showed a 9-point improvement in their symptoms on a standardized assessment for Parkinson’s disease, and those who received the high dose gained 23 points. The assessment measures individuals’ daily life activities, pain levels, sleep and eating. Agnete Kirkeby is a Stem-cell scientist who is involved in a European trial and says that the results warrant larger trials despite the fact that the metric is subjective.
Morphological and neurotoxic effects in the death of iPS cell embryos in post-mortem imaging and surgery: A multi-stage crossover study
Yamanaka discovered in 2006 that adult cells could be reprogrammed into embryo-like state, capable of being any kind of tissue. In 2012 Yamanaka won a gold medal at the London Olympics, and became a household name due to the iPS cells. They have become a symbol of the country’s global scientific aspirations.
Three individuals received up to 5 million cells and 4 received up to 11 million cells, of which 150,000 and 300,000 cells, respectively, were expected to survive. “This low survival rate is a big problem that needs to be solved,” says Jun Takahashi, a neurosurgeon at Kyoto University in Japan, who led the trial. Participants were given immune-suppressing drugs for 15 months.
No serious adverse events were reported for all seven patients subjected to safety assessment. The graft size increased over time with the images. However, no tumorigenic overgrowth was identified, as evidenced by the absence of 18F-FLT uptake, a marker of cellular proliferation, which was indirectly supported by results from the transplantation experiment using the same donor cells into PD model rats. Histology showed no evidence of overgrowth, less than 1% of cells were Ki-67 positive. A study has claimed that the increase in donor volume is due to the spread of the grafted cells. While such effects may also apply to our trial, further confirmation through long-term follow-up and post-mortem histological examinations is necessary. Similar adverse events were seen with chronic DA replacement medication, tacrolimus administration and brain surgery. Neck stiffness and painful dystonia in the right upper limb were noted in PD01 during the drug-on state, a phenomenon possibly related to the grafts. Tacrolimus- and surgery-related adverse events were manageable and reversible.
There were discrepancies in the scores between the Hoehn–Yahr stage and the part III scores. The Hoehn–Yahr stage emphasizes postural instability and mobility issues, whereas the MDS-UPDRS part III offers a more comprehensive evaluation of major motor symptoms in PD. Consequently, improved postural stability and mobility may account for the greater improvement in the Hoehn–Yahr stage compared with changes observed in MDS-UPDRS part III scores of this study.
The potential of donor iPS-cell-derived transplants: a case study from Kobe City Eye Hospital, Japan, and the Vision Care Biotechnology System
Scientists launched clinical trials and start-up firms. Large companies made more money in manufacturing hubs. A big amount of patients from Japan and abroad will be arriving at medical facilities. “Regenerative medicine in Japan is moving very dramatically,” says Masayo Takahashi, an ophthalmologist at Kobe City Eye Hospital and president of the biotechnology company, Vision Care. In 2014, she became the first to treat someone with cells derived from iPS cells.
These organizations are working in a system, launched in Japan in 2013, that permits ‘regenerative-medicine products’ to be licensed for temporary use if early-stage clinical trials show that the products are safe to use and have potential for clinical benefit. This system allows products to be rolled out without completing phase III randomized-controlled clinical trials — which are generally considered to be the ‘gold standard’ test around the world. However, after conditional approval, evaluations do continue, and both safety and efficacy must be shown conclusively or the product is withdrawn.
But those approvals are not yet in hand, treatment costs are high, large trials showing clear clinical benefit have yet to materialize, and concerns about safety could still sap the public’s willingness to try this treatment. The potential of the cells and the limits of their development are what we are realizing.
Yamanaka promised that his iPS cells wouldn’t be subjected to a bioethical stand-off that had threatened the future of stem cells. Because production of iPS cells doesn’t require the destruction of human embryos, they were considered ethically less fraught. Furthermore, because they could be made from the cells of the person in need of treatment, they promised to offer transplantable tissues without the need for immune-suppressing drugs.
In November, Kohji Nishida, an ophthalmologist at Osaka University, and his colleagues published the results of donor iPS-cell-derived transplants into four individuals for whom those natural cornea-building stem cells had been depleted — a condition that results in corneal scarring and vision impairment. Three of them saw sustained gains in vision3.
It was a procedure that was hard to do. Self-derived, or ‘autologous’, cell therapies are time-consuming and expensive to make, and the large cell-sheets that researchers crafted for implantation required intrusive surgery. Takahashi says she chose this approach to ensure the highest chance of clinical benefit — to demonstrate to the world what was possible. It was designed to be the best treatment.
The difficulties might come down to the retina’s natural resistance to regeneration. The clear covering of the eye that lets light in is also maintained by a pool of stem cells, which might benefit from cell therapies.
A man’s perspective on Japan’s fast-track system for the development of iPS cells: Managing the risk for patients with rare conditions
Nishida has set up a company called Raymei, which will launch a larger trial in three years. “The next clinical trial is pivotal,” he says.
The hope of iPS cells is to restore nerve tissue, but it has been a challenge. Jun Takahashi, husband to Masayo, has an office lined with statues of elephants and an imposing, life-sized set of navy-blue samurai armour, “just to encourage my lab”, he says.
But, unlike his wife, he has not set up a company to develop the technology for manufacturing the cells and conducting the surgery. He’s transferred that information to the Osaka-based Sumitomo Pharma. “As a scientist, I am kind of satisfied,” he says. He’s concentrating on developing cell therapies for stroke.
Others are less concerned about Japan’s fast-track process for conditions that are rare or have few other treatment options. “In order to move this field forward quickly, you’re going to have to have an element of risk,” says Svendsen. They are putting in place regulations in Japan and that has been pretty sensible.
Companies can offer the treatments, with costs mostly covered by the national health system. They need to collect data on their safety and efficacy to get full clinical approval.
The fast-track system’s safeguards are working according to one interpretation. The candidate treatments, which needed more time in clinical trials, were clearly needed. The failure to achieve the desired level of efficacy meant that patients experienced false hope, and because treatments grantedconditional approval are paid for through Japan’s public health-insurance system, taxpayers were left with an unnecessary bill.
A Two-Armed Robot for Macular-Degeneration Research: Preliminary Results from Initial Clinical Trials and a Comparison With a Clinical Trial
Masayo Takahashi has chosen a more portable manufacturing model for her macular-degeneration treatments: a white, muscular-looking, two-armed robot. Powered by machine learning, it checks in on cells’ progress as they are prepared for transplant through a microscope. In 4 months, it can produce enough cells for more than 800 individual treatments.
Such work has the potential to transform lives, but it is important that these therapies do not move into the clinic too quickly. Researchers must be allowed to complete their studies as much as they need to.
Both studies, which are reporting the results of early stage clinical trials, show that the interventions were safe and that the recipients experienced measurable improvements in typical symptoms.